Devil or angel, I can't make up my mind
Which one you are I'd like to wake up and find
These are the opening lyrics of Bobby Vee’s 1960 recording of his first song to break into the top 10..
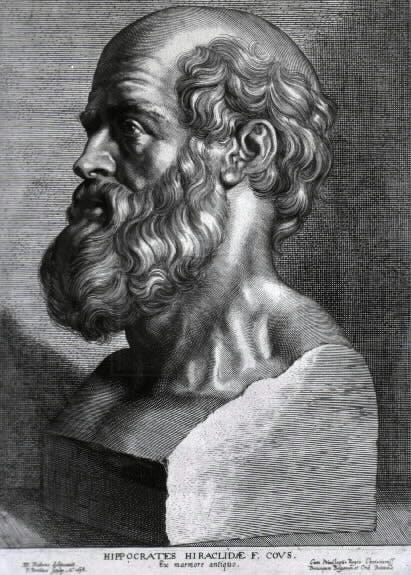
The Oath of Hippocrates has been associated for millennia with individuals entering the profession of medicine. For many reasons, it has been “updated” to be relevant for modern times. This is a portion of the oath taken from Bulger, R. A dialogue with Hippocrates and Griff T. Ross, M.D. In Bulger R, ed. In Search of the Modern Hippocrates. Iowa City: University of Iowa City Press; 1987:253:
I shall do by my patients as I would be done by; shall obtain consultation whenever I or they desire; shall include them to the extent they wish in all important decisions; and shall minimize suffering whenever a cure cannot be obtained, understanding that a dignified death is an important goal in everyone’s life. (emphasis added)
I practiced clinical medicine from 1975 to 2017. Forty-two years is a long time.. I was both legally and morally bound to provide Informed Consent for any of the surgical procedures or medical treatments I recommended. This meant that I was bound to explain the risks, benefits and alternatives of the proposed treatment and then allow the patient, or their legal guardian, to decide on the course of action they wished to follow. I could be sued for malpractice if I did not follow those rules. Many physicians were and fortunately I never was one of those.
Recently that same moral, ethical and legal requirement has been discussed in the medical literature with troubling dissimilar slants. Medscape, a publication linked to Big Pharma in the past, reported that Drs. Pierre Kory and Paul Marik were stripped of their board certifications by the American Board of Internal Medicine for spreading “misinformation”. However, when one looks at the actual “misinformation”, it sounds a lot like they were following the dictates of the updated Oath of Hippocrates quoted above! They were attempting to deliver true Informed Consent to their patients by giving them complete information on possible treatments for COVID and the risk/benefit ratio of receiving the mRNA agents and not just the articles that arguably were designed with the conclusion already decided.
Contrast what happened to them, and countless numbers of other physicians who did the same thing, with this recent editorial in JAMA: Oaths, Conscience, Contracts, and Laws—The Gathering Storm Confronting Medical Professionalism. You may not be able to view this as it is behind a paywall, so let me give some relevant quotes:
The bond between physicians and their patients has long been considered a unique, even sacred, relationship sealed with publicly professed oaths. Historically, an essential and ubiquitous component of physicians’ oaths and their related ethical codes is the promise to place patients’ interests above any others, including their own. This is a high bar, but it is the bar physicians swear to meet when entering the profession.
The editorial goes on to explain that in some states, laws have been passed that the authors consider to be in error as they prioritize physicians’ conscience over patients’ interests:
But for physicians, they also represent an attack at the heart of professionalism: namely, the right of physicians to establish medical standards of care and their related obligation to put patient interests first when doing so…
What should be done? First, physicians should recommit to their sworn oaths and codes of ethics that prioritize the patient as the center of care...
As a profession, physicians must vigorously defend their authority to make medical decisions with their patients’ interest at heart. Where the authority to put patients first has already been lost, physicians should work with other groups, including patient advocacy groups, to help regain it. In the current environment, working to recenter medical care around patients’ interests can be difficult or even dangerous, but it is the only path forward if physicians hope to remain a true profession. (emphasis added)
The authors of the editorial are talking about the duty to override any laws seeking to limit abortion or “gender affirming” care…but why only in those cases? isn’t this precisely what Drs. Kory and Marik and hundreds of others were doing when they exercised their right and duty to prioritize the patient as the center of care?!
You see the problem here: Is this editorial, and by extension JAMA and organized medicine that it represents, actually prioritizing the patient, or their own ideology? Is it logically and morally consistent to champion the patient’s right to make decisions about their own care only in some situations and not in others?
I would agree with one thing in the editorial: The answer to this question will indeed be the only path forward if physicians hope to remain a true profession.
Unfortunately, in my estimation we are on the wrong path right now. And, ironically, it appears that the American Board of Internal Medicine, the very organization that decertified Drs. Kory and Marik, may agree!
This transcript of an interview with Rich Barron, MD, the CEO of the American Board of Internal Medicine, is amazing. All of you should follow the hyperlink and read it and draw your own conclusion. This is a taste:
I think many of us in health care think we have trust because we have good intentions. And frankly, it's not news to your viewers that the American Board of Internal Medicine lost trust with lots of our diplomats. And we assumed, oh, we've got that. We have the right intention. We have the right people. We have qualified people. Why would people distrust us?
And people did. And it was because we had neglected the relationship with the doctors that we were serving. And we had assumed that, of course, they think we're on the right side and, of course, they think we have their best interests at heart. And it turned out that we had failed organizationally to build the connections we needed to build to be successful.
And part of how the ABIM Foundation decided to go into this direction was we realized that ABIM was not alone within the health care universe of believing that because we had expertise, because we had experts, because we had science, of course, people will trust us. And in fact, science and expertise is not enough, not close to enough.
The American Board of Internal Medicine even has an initiative to build trust. Go to the website and look at it. As yourself: is this about the message or the messaging? Is it written for the benefit of the patient or the physician?
From my perspective, building trust is really quite simple: be consistent and tell the truth. When you make a mistake, admit it. Follow this:
I shall do by my patients as I would be done by; shall obtain consultation whenever I or they desire; shall include them to the extent they wish in all important decisions; and shall minimize suffering whenever a cure cannot be obtained, understanding that a dignified death is an important goal in everyone’s life.

Excellent piece, Dr Gonnering! Sadly, medicine has been corrupted, with too many physicians more focused on protocol and ideology than actual care of patients. When I was a practicing NP, informed consent was always at the forefront when discussing medications, biologics, procedures, or research with patients. That requirement seems to have disappeared, and I find that equally disturbing and sad. Thank you for addressing this.
Trying to restack-error occurring.
Thank you for this most needful article.