One of the reasons healthcare, particularly medicine, is losing credibility the past 4 years is that it is caught in The DEI Attractor Well. Let me explain:
Healthcare is a Complex Adaptive System. It is made up of multiple interdependent agents (people and organizations) under loose central control where the starting point is critical, and order ideally emerges from interactions between those agents and the underlying system. Optimally, it behaves much like a jazz ensemble or the interplay between the guitar and banjo in the classic movie Deliverance. It can be wonderfully creative and innovative, but when stifled by imposed order, it becomes stale.
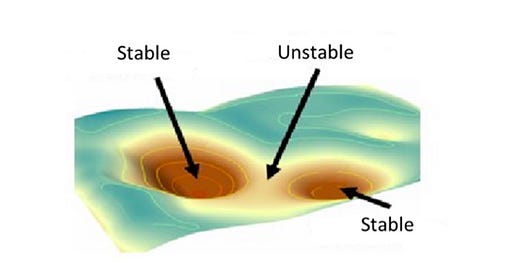
Complex Adaptive Systems move much like a marble on a slightly inclined plane of sheet metal that is jiggled. Driven by gravity, along the way the marble can stop in slight indentations. Those indentions act as an attractor, for if the marble comes close enough it is captured by the well. They act as areas of stability:
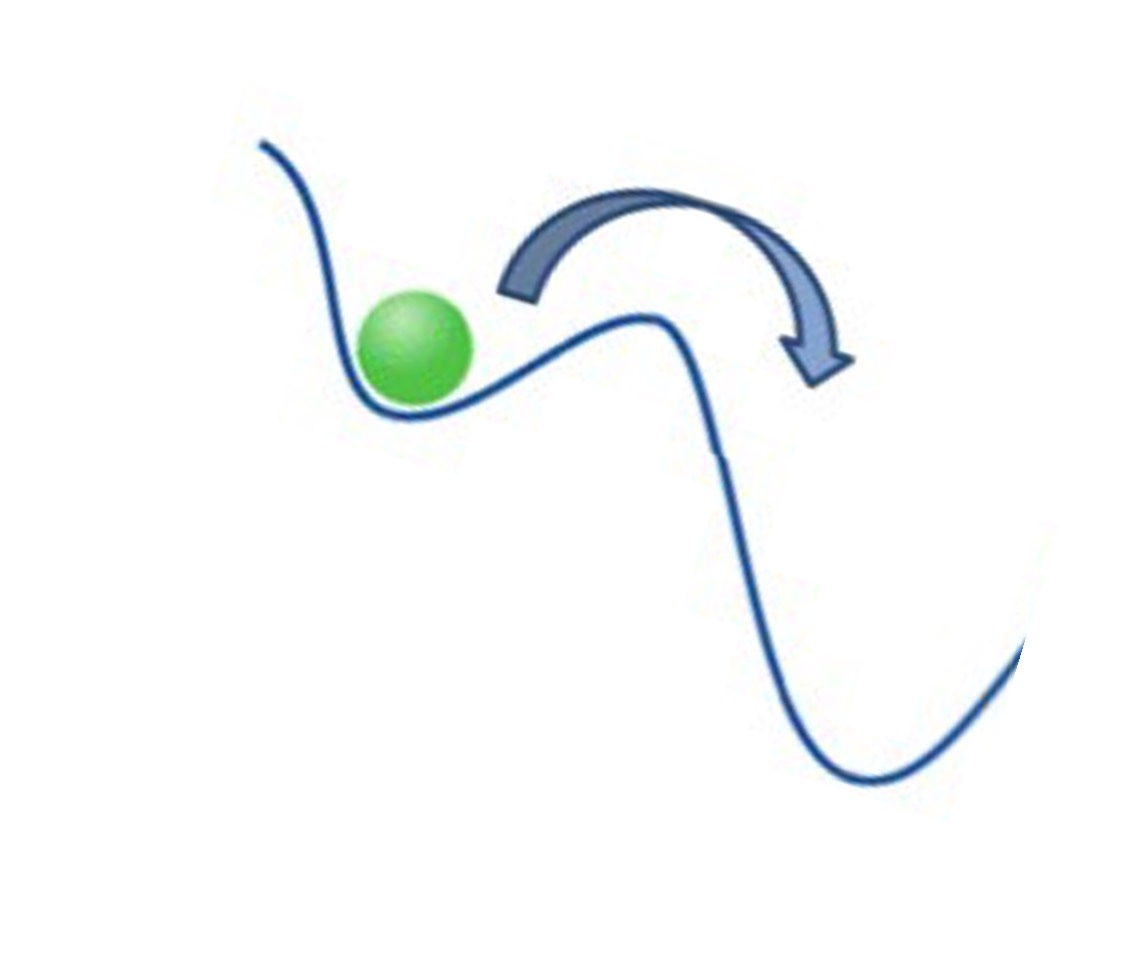
Once captured by the attractor, increased force over and above the periodic jiggle is necessary in order to free the marble:
If the attractor is strong, and the well deep, greater force is needed. The DEI well into which medicine has fallen is wide and deep and the negative effects are continuing to ripple through society.
As is often the case, the construction of this attractor well took some time and was paved with good intentions. In 1999 the Accreditation Council on
Graduate Medical Education (ACGME) endorsed a change from a structure-based graduate medical education to one based on actual competency. It was a huge step forward. Instead of just spending a set amount of time learning subsections of a residency program, actual competencies in the areas were tested. These Clinical Competencies were:
· Patient Care
· Medical Knowledge
· Interpersonal and Communication Skills
· Professionalism
· Practice-Based Learning and Improvement
· Systems-Based Practice
In 2011, the American Association of Medical Colleges (AAMC) developed similar core competencies for entering medical students:
· Service Orientation
· Social Skills
· Cultural Competence
· Teamwork
· Oral Communication
· Ethical Responsibility to Self and Others
· Reliability and Dependability
· Resilience and Adaptability
· Capacity for Improvement
· Critical Thinking
· Quantitative Reasoning
· Scientific Inquiry
· Written Communication
· Knowledge of Living Systems
· Knowledge of Human Behavior
In 2013 a recommendation was made to include “Cultural Competence” in order address any inequality of care based upon diverse backgrounds. By 2023, the list of core competencies for entering medical students had been significantly expanded to:
· Professional Competencies
o Commitment to Learning and Growth
o Cultural Awareness
o Cultural Humility
o Empathy and Compassion
o Ethical Responsibility to Self and Others
o Interpersonal Skills
o Oral Communication
o Reliability and Dependability
o Resilience and Adaptability
· Science Competencies
o Human Behavior
o Living Systems
· Thinking and Reasoning Competencies
o Critical Thinking
o Quantitative Reasoning
o Scientific Inquiry
o Written Communication
A standard application administered by The American Medical Application Service (AMCAS) is used by students applying to medical schools in the United States. Detailed tools and tutorials on the process are found on the AMCAS website.
The AAMC is completely unambiguous in stating their orientation is directed primarily at rooting out perceived systemic racism in our medical apparatus. In addition, the AAMC includes a very informative “Inspiring Stories” on their website giving a look into 93 applicants who made a difference and were successful in their application. These will be encouraging to those who are worried that the majority of successful applicates are straight white males.
The important question, however, is how do the admissions committees use this information to evaluate applicants? Do they pay attention to the afore mentioned Core Competencies? If they do, how do they score the individual elements? How do they weight them? What do they understand to be Cultural Awareness and Cultural Humility?
With the death of George Floyd and the massive outpouring of protest in the summer of 2020, the DEI attractor was significantly enlarged in all of academia. The deleterious effects of DEI in our most prestigious academic institutions have been recognized. However, the effects in healthcare are less well-publicized. A few articles, such as the decline of medical education at UCLA, have surfaced.
That may have finally changed. This past week a monumental study by Do No Harm took direct aim at the AAMC and its primary focus on DEI. The 80-page report (in the hyperlink) is devastating. It meticulously catalogs the descent of the AAMC from an institution focused on merit to one primarily dealing with Social Justice. As the problem is so pervasive, it recommends drastic action:
Because the AAMC has vast financial and strategic resources to
maintain its current trajectory, substantial measures must be
taken to reverse the destructive course the organization – and,
therefore, medical education – is on. With the degree of influence
the AAMC has on policy and legislation, an even stronger offensive
is needed to counter their efforts. States must continue to take
action to remove DEI from their public institutions, but federal
legislation such as the EDUCATE Act and the End Woke Higher
Education Act is necessary to sever the funding pipelines that
allow the perpetuation of divisive and discriminatory practices in
the country’s medical schools.
To return to the language of Complexity Science, DEI has gone beyond acting as a huge Attractor Well and an area of merely aberrant stability to one transforming the emergent order of the Complex Adaptive System of medical education to an imposed order where the agents have virtually no meaningful contribution to the direction. Positive feedback is impotent and learning lost. It converts the creative energy of the Complex Domain into Chaos. It is a transformation into Lysenkoism in medical education. We cannot let that happen…..


DEI, or DIE, as Dr. Tamzin Rosenwasser of AAPS prefers, has absolutely no place in medical education, or in Medicine. As our dear colleague and friend, the late Dr. Marilyn Singleton said, doctors are the least racist group and systemic racism doesn’t exist in Medicine. Who, besides Do No Harm and the Association of American Physicians and Surgeons is pushing back against this nonsense?
Our major universities have become so enthralled with DEI that their numbers of staff rivals the academic staff at some universities, such as the University of Michigan, a once proud academic institution. Undoubtedly this includes the medical schools. All races have candidates who meritorially qualify for entrance into medical schools, and they should be the ones who are accepted. The public, in the past, had trusted their lives to these people. That is no longer the case. I’ve read that only 40% now trust physicians. The COVID debacle has awoken them. A good step forward is for DEI to DIE.